What is the health situation in Zimbabwe and what are the consequences of the pandemic for the population? What do the Covid 19 restrictions mean for the rampant sexual violence against girls and women in South Africa and what is the NGO LifeLine doing about it? The big interview with Tayson Mudarikiri (36) in Harare, project coordinator of terre des hommes switzerland for Zimbabwe and South Africa.
Tayson, how are you?
Quite good. I hope our children don't interfere with our video call. They are both homeschooling and they may well "visit" me in my office in between.
Your children don't bother you at all. How do you manage the home office in Harare?
If you are working on something that requires a lot of concentration, you can be distracted. On the other hand, it's good if the children have questions about their homework and you can help them briefly. We're lucky, my wife isn't working at the moment. So she can take over at home and I can do my work.
You were infected with Covid-19. How is your health now?
I'm doing quite well again. The whole thing was stressful, not because of the symptoms, which were limited. But it would help if I could say that was the specific moment of infection.
What happened and how did the disease progress?
We spent the Christmas vacations together with a family friend. That was nothing out of the ordinary. After the first hard lockdown in Zimbabwe in spring 2020, there were very few Covid-19 cases for a long time and transmission rates were low. Our country was quite open. On Christmas Eve, the father of the other family was not well. He is 40 years old and healthy. However, he has diabetes and had already been in hospital for a total of 30 days in the two months before the festive season due to his chronic illness. He suddenly became very weak and had difficulty breathing. So I drove him to the nearby hospital, where he spent four days and was tested for Covid-19 - negative.
So there's no need to worry.
Well, a little later I developed a high temperature. The next day it was gone again, but I got a headache, which wasn't too worrying. The next day I felt better again, I just felt very weak. When this weakness was still there a week later, I went to the doctor. She looked at me and knew it was Covid-19, which a test confirmed. I was given medication and that helped. The coronavirus took its toll on my strength, but overall it wasn't bad. I've been feeling better every day for a week now and I drink a lot of ginger tea. (Laughs) It's hard to say when and where I caught it. But it's likely that it happened when I visited my colleague, the father of the family friend, in hospital.
Has your family also been tested for Covid-19?
A corona test costs a fortune, 60 US dollars. That's 240 dollars if all four of us were to get tested. We do what most families do in the case of Covid-19, we make sure it stays within the family and make sure we protect ourselves from each other.
We don't have much space at home. My wife lives with the children in their room and I stay in my parents' bedroom all the time. We also adhere to the recommended hygiene measures. We have drastically reduced our social contacts. My wife had a bad cough for a few days, but it disappeared again. If any of us develop typical symptoms in the next 14 days, we will take a virus test.
Is the Zimbabwean government planning a vaccination program for the population?
Officially, no one has yet been vaccinated in Zimbabwe because the government has not ordered a vaccine. As far as I know, we are due to receive around 3 million vaccine doses in the near future via the African Union and for around 15 percent of the population. There is currently no national plan as to who should be vaccinated and which groups should be prioritized.
What is your own policy on vaccination?
I will get vaccinated if there is a government plan. But I haven't had any worrying symptoms and my health is fine. However, health workers should definitely be vaccinated as they are the most exposed. Priority should also be given to the elderly and other vulnerable groups, as well as children. I think the model in Zimbabwe will be: Those who can afford it will get vaccinated and it will certainly require international vaccination donations. But the big question of who can afford a Covid-19 vaccination remains.
There are many misconceptions about viruses and vaccination - not just in my country, but worldwide. Personally, I can't relate to such attitudes, I stick to public health interventions. There needs to be a lot of information and education about how vaccinations actually work and what they can do.
What resistance is there to a Covid-19 vaccination?
The biggest problem for Zimbabwe and for Africa in relation to the vaccination issue is the link with religions. We have a new wave of "leaders of change", magical priests and also Christian leaders who are proclaiming, I am not taking this vaccine because there is a conspiracy behind it. Such leaders and their fundamentalist religious rites have millions of followers in Southern Africa. That scares me from a public health perspective. In Zimbabwe, the situation is somewhat different and there are fewer barriers to scientific information. Because practically every person has been vaccinated by the health system, against polio, tuberculosis and so on. What it takes for people to get vaccinated against Covid-19 is for the government to say: you already know about vaccination, now it's just a new, unprecedented phenomenon.

Apart from the virus issue, what everyday worries do people in Zimbabwe have?
That there is enough food on the table. Over 90 percent of the population work in the informal sector. In contrast to the health sector and employees in mining and agriculture, they are currently not allowed to work. For them, every day in lockdown is a day without income. So people are going outside anyway, as they did during the first lockdown in April 2020, because it's the only way they can feed their families. It is only a small minority like us who can continue to work as before and receive a wage.
So it is economic worries that are plaguing people, and not concerns about their own health and that of others?
It's not quite that simple. If you look on social media or talk to people, you see: Everyone knows someone who has Covid-19 or is struggling with health complications because of it and the other problem is, how do you get adequate help if you fall ill? So the message has to be: people, take this seriously, because Covid-19 can kill people.
The pandemic has led to an increase in gender-based violence against women and children.
Gender-based violence or GBV is a permanent problem, not only in southern Africa, but in all regions of the world. However, the situation is particularly bad in South Africa. Key factors are social and cultural norms in a patriarchal society. While they do not necessarily promote GBV directly, they do allow for certain forms of sexualized violence against an individual. The patriarchal system gives men absolute power. Including power over the bodies of their sisters, wives and partners. It is very difficult to stop GBV in patriarchal societies. If the decision-makers in the judiciary, politics, administration or community level are all men, you reinforce this norm against women and thus also sexual violence against them.
How does the GBV standard manifest itself in concrete terms?
When you get married in Africa, you pay a bride price. This means that the woman is accepted into the family of the man who has absolute authority over her. Many men then feel they have the right to rape their wives, because she belongs entirely to him and he has paid a price for her. "You are at my disposal whenever I need you."
In order to break with this inhumane practice, we need to raise awareness of the rights of women and children (Sexual and Reproductive Health and Rights SRHR, editor's note). Most men are not even aware that they are raping their wives. In the last 20 to 30 years, there has been a wave of initiatives and official regulations in Africa to raise awareness and prevent GBV. But in many places they are not enforced because the institutions are too weak. In Zimbabwe, for example, there is a national gender commission, but it is understaffed and has too little budget to ensure that these requirements are actually implemented. This gives the impression that such state commissions are only being set up to satisfy the growing need for institutions to deal with these issues.
Sexual violence against women and children is increasing in the context of the coronavirus crisis.
Yes, reliable figures on the situation in Zimbabwe are currently being collected. A report from the end of 2020 by our partner organizations working in schools shows: There are some girls who did not come back after school reopened because they are pregnant. Another problem is the poor connections in public transport, which are being curbed again due to the lockdown. This is a major problem, because anyone who has been raped usually needs transport to the nearest health center. The biggest challenge is: how can the most vital services be maintained for those who urgently need them?
There is a big difference between the GBV and HIV services: For the latter, we have found ways to get the drugs from the hospital to the young people in the community. But we don't know who has been raped and where the survivors are. Most of them were raped at home. You must first remove the rapist from the house and take the survivors to the health services before you can follow up and counsel them.

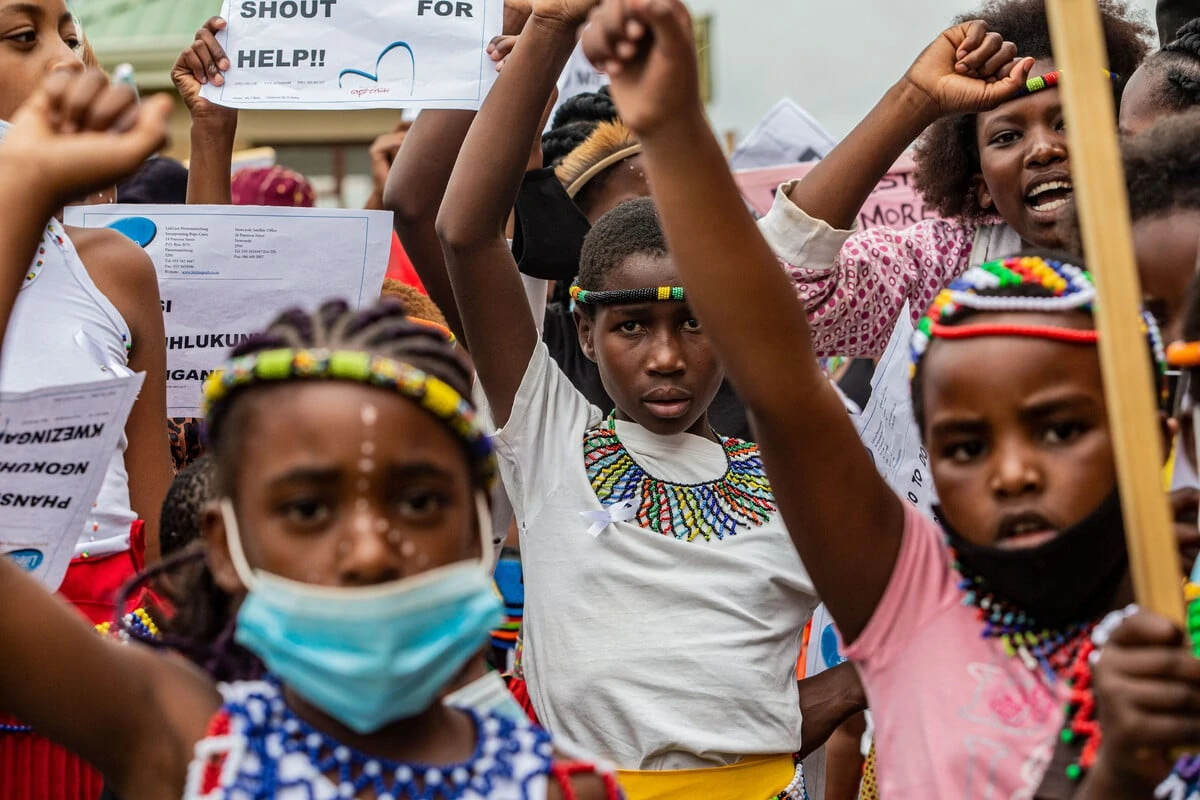
While terre des hommes switzerland in Zimbabwe works on a range of SRHR and health issues, has LifeLine in South Africa a clear GBV profile. What characterizes our partner organization in KwaZulu-Natal?
LifeLine shows what a GBV program needs to look like to be sustainable. LifeLine works on two tracks, firstly in prevention and secondly in helping and supporting survivors so that they have hope and can lead their lives as free as possible from their traumatic experiences. In other words, LifeLine's approach is holistic. We have staff who work in the community every day. They are available for practical advice and to answer questions related to GBV.
Recently, our South African partner organization has also been working in the area of cultural and social norms and thus on structural violence against women and children.
Our South African partner organization works with the target group of men in decision-making positions at community level, which is unique. LifeLine works with them on the question: How can we better protect women and ensure that all community members are aware of SRHR? It's about working with the men who set the tone to create places where perpetrators are held accountable if they don't treat their wives properly.
There may be the most exemplary national gender guidelines on paper - what counts is that the actors in the communities ensure that they are actually applied. A community leader who takes it for granted that a man will rape his wife is fomenting a climate of sexual violence rather than helping to curb and prevent it. It is important to ensure that the police comply with the law. Information and education on the rights of women and children are key. School management and teachers and healthcare staff in outpatient clinics or hospitals must also be aware of this SRHR and act accordingly.
What is LifeLine doing to ensure that the perpetrators are brought to justice?
You mention an important key factor, the South African justice system. Practice shows that even if someone is arrested for GBV, the justice system is so corrupt that in many cases the perpetrator is not prosecuted. LifeLine therefore spoke out strongly on this issue during the 16 Days against Violence against Women last November and received a lot of media coverage. There was even an interview on the national TV channel.
Interview: Anna Wegelin
More about our focus area Health for Sexual and Reproductive Health and Rights (SRHR) and against Gender-Based Violence (GBV) here


